We may earn money or products from the companies mentioned in this post. This means if you click on the link and purchase the item, I will receive a small commission at no extra cost to you ... you're just helping re-supply our family's travel fund.

Travel can be thrilling, eye-opening, and deeply rewarding, but it also exposes travelers to health risks that are easy to underestimate. In certain parts of the world, climate, infrastructure gaps, population density, and wildlife interaction create conditions where serious infectious diseases still thrive. These destinations are not off-limits or inherently unsafe, yet they demand careful planning, medical awareness, and preventive action. Understanding the real risks along with the numbers behind them helps travelers make informed decisions and stay protected without sacrificing the experience.
1. Democratic Republic of the Congo

The Democratic Republic of the Congo remains one of the most disease-vulnerable countries due to vast rainforests and limited healthcare access. Since 1976, over 15 Ebola outbreaks have been recorded here, with fatality rates ranging from 25% to 90% depending on strain and response speed. Malaria accounts for nearly 40% of outpatient visits, while cholera cases often exceed 20,000 annually. Travel beyond major cities significantly increases risk, as rural clinics may be days away. Fever, dehydration, or minor infections can escalate quickly without treatment, making preparation and rapid response critical.
2. Nigeria

Nigeria’s large population of over 220 million people creates ideal conditions for disease transmission. The country reports 100,000+ malaria deaths annually, the highest global total. Lassa fever causes 3,000–5,000 deaths each year, often linked to rodent exposure in urban housing. Yellow fever outbreaks still occur despite vaccination campaigns, with thousands of suspected cases yearly. While private hospitals in cities like Lagos are advanced, rural regions face shortages of doctors and equipment. Travelers moving between urban and remote areas must take preventive medication and vaccination seriously.
3. India

India’s diverse climate and dense population contribute to recurring outbreaks of infectious diseases. Dengue alone causes over 100,000 reported cases annually, with numbers likely higher due to underreporting. Tuberculosis affects nearly 2.8 million people each year, including drug-resistant strains. Seasonal monsoons increase waterborne illnesses like typhoid and hepatitis A. Although healthcare quality varies widely, delayed treatment is a major risk factor. Most traveler infections stem from contaminated food, unsafe water, or mosquito bites rather than extreme exposure.
4. Brazil

Brazil’s tropical and subtropical regions are hotspots for mosquito-borne illnesses. Dengue cases surpassed 1.6 million in recent peak years, while yellow fever outbreaks have caused hundreds of deaths in forested states. Zika, though rarely fatal, poses severe risks for pregnant travelers. Malaria remains active in the Amazon basin, with over 130,000 cases annually. Major cities offer strong healthcare, but rural and jungle areas do not. Risk rises sharply during rainy seasons when mosquito populations surge.
5. Uganda
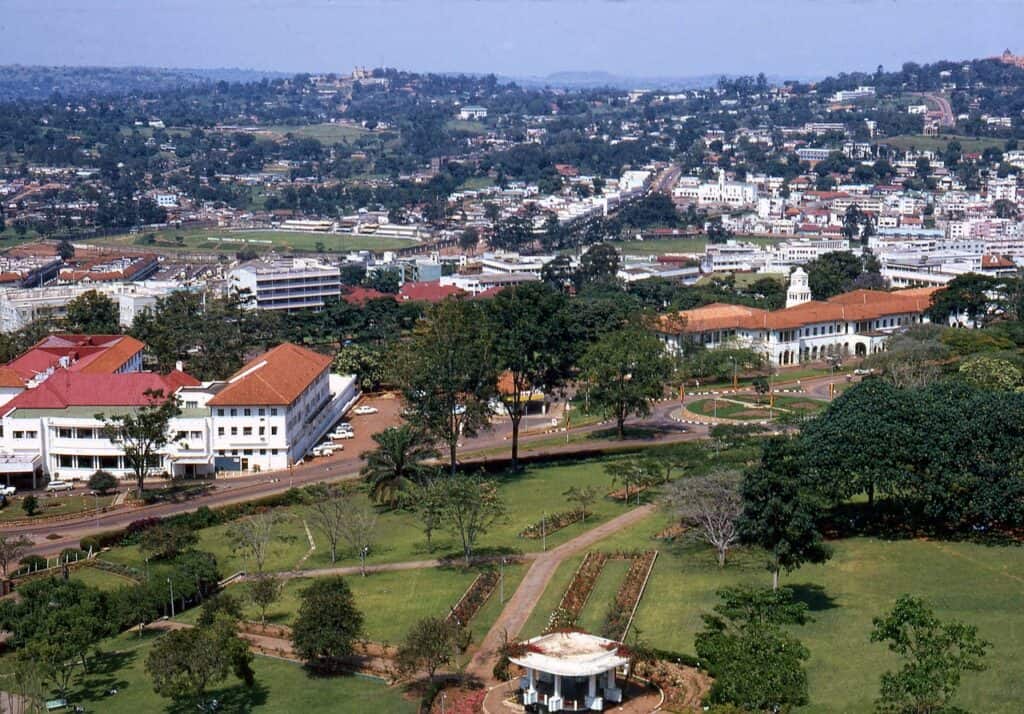
Uganda’s location near dense forests makes it vulnerable to viral hemorrhagic diseases. Ebola and Marburg outbreaks, though sporadic, have recorded fatality rates of 30–80%. Malaria is endemic, responsible for 30–50% of hospital admissions nationwide. Rural travel increases exposure due to limited diagnostic facilities and delayed treatment. Uganda’s wildlife tourism adds another layer of risk, particularly near bat-inhabited caves. Early medical attention for fever is crucial, as symptoms often mimic common flu initially.
6. Haiti

Haiti continues to battle long-term public health challenges worsened by natural disasters. Cholera outbreaks since 2010 have caused over 800,000 infections and nearly 10,000 deaths. Tuberculosis rates remain among the highest in the region, with 130 cases per 100,000 people annually. Limited access to clean water amplifies risk even for short-term visitors. Dehydration from gastrointestinal illness can become life-threatening without prompt care, making safe water practices essential.
7. Papua New Guinea

Papua New Guinea’s isolation and rugged terrain complicate healthcare delivery. Malaria affects over 1 million people annually, while tuberculosis incidence exceeds 430 cases per 100,000, among the highest globally. Medical evacuation is often the only option for severe illness. Rural villages may lack electricity, let alone advanced care. Travelers engaging in trekking, research, or volunteer work face higher exposure risks due to prolonged stays and limited sanitation infrastructure.
8. Sierra Leone

Sierra Leone is still rebuilding trust in its health system after the Ebola crisis, which killed over 3,900 people locally. Malaria remains the leading cause of death, responsible for nearly 25% of fatalities nationwide. Lassa fever and cholera outbreaks occur intermittently, especially during rainy seasons. Healthcare access outside Freetown is limited, and early symptoms are often overlooked. Prompt medical evaluation for fever can be lifesaving in this environment.
9. Bangladesh

Bangladesh’s dense population of over 170 million people combined with seasonal flooding fuels disease spread. Cholera causes tens of thousands of cases annually, while dengue outbreaks have exceeded 300,000 cases in peak years. Typhoid and hepatitis E remain persistent threats linked to water contamination. Hospitals in major cities are capable, but rural care is uneven. Travelers are most at risk from unsafe food, untreated water, and poor hand hygiene rather than direct contact.
10. Venezuela
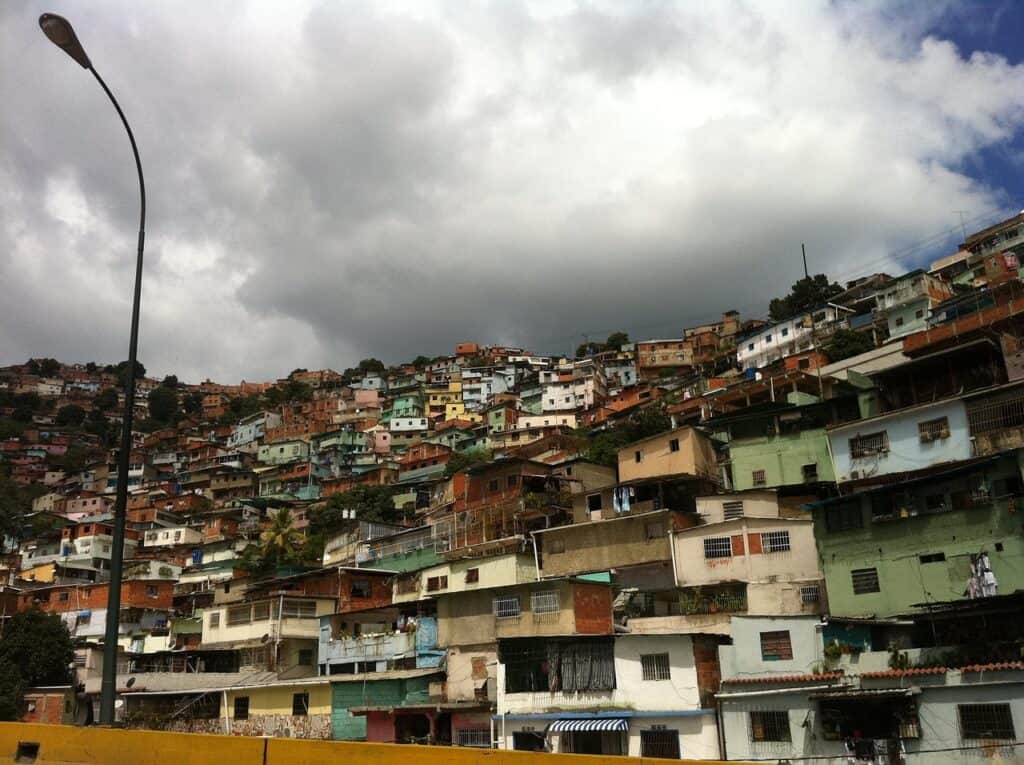
Venezuela has seen the re-emergence of diseases once considered controlled. Malaria cases rose from under 50,000 in 2000 to over 300,000 annually in recent years. Measles and diphtheria outbreaks have also returned due to vaccination gaps. Medicine shortages and inconsistent reporting complicate treatment. Travelers may struggle to access basic care in emergencies, especially outside Caracas. Preparation and avoidance of high-risk regions are essential.